Abstract
Introduction
Myeloid-derived suppressive cells (MDSCs) represent a collection of myeloid-lineage immature cells owning immunosuppressive ability to facilitate tumor growth and can be phenotyped into two major groups: monocytic MDSC (M-MDSC) and granulocytic MDSC (G-MDSC). Earlier studies demonstrated the association between M-MDSC and prognosis in lymphoma patients. Triggering Receptors Expressed on Myeloid cells 2 (TREM-2) is a transmembrane glycoprotein and well-known to polarize macrophage to M2-like phenotype presenting anti-inflammation properties. Given that both the macrophage and M-MDSC belong to monocytic lineage, we wondered if TREM-2 was also expressed on M-MDSC cell surface and tried to elucidate the clinical impact of surface TREM-2 on M-MDSC derived from patients with newly-diagnosed and treatment-naïve non-Hodgkin lymphoma (NHL).
Methods
This was a prospective observational study conducted in a tertiary medical center (Taipei Veterans General Hospital) in Taiwan. Adult patients with newly-diagnosed and treatment-naïve NHL were eligible for enrollment from May 15, 2019 to February 28, 2021. Patients with HIV infection or other concurrent malignancies were excluded. The Mann-Whitney U test was used for quantitative data, the Kaplan-Meier estimate and log-rank test for survival data, and Cox regression models for hazard ratios (HRs).
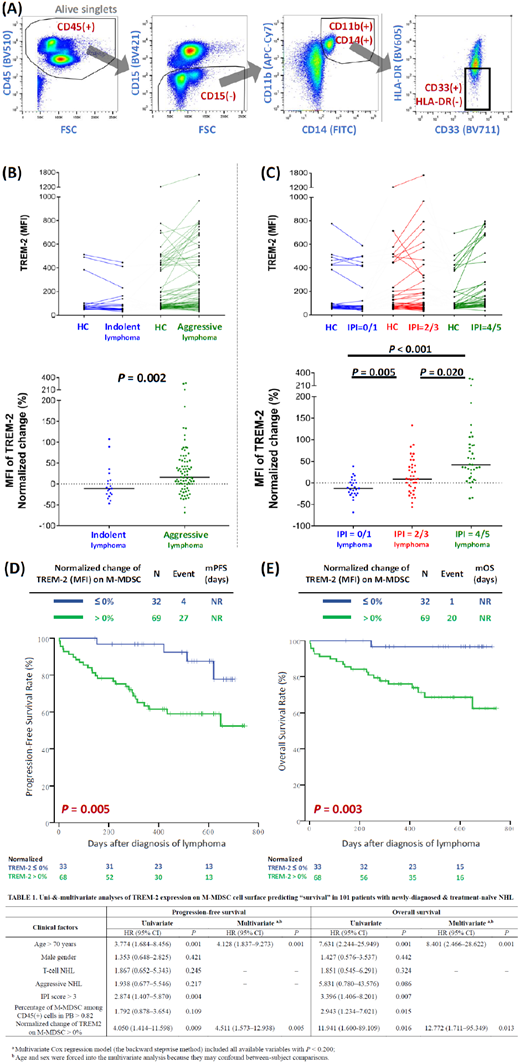
Human M-MDSC (defined as CD14 + CD11b + CD33 + HLA-DR - CD15 - cells, Figure A) was obtained from freshly isolated PBMC before initiating any treatment, including steroid. To increase inter-experiment reproducibility, the peripheral blood (PB) from the principal investigator (Hao-yuan Wang) was utilized as an internal control (Healthy Control), and every patient's blood sample was paired to the Healthy Control at the same performance of flow cytometric analysis to calculate the normalized MFI change of TREM-2 as the following: (Patient's TREM2 MFI - Healthy Control's TREM2 MFI) / (Healthy Control's TREM2 MFI) x100 %
Results
One hundred and one adults with newly-diagnosed and treatment-naïve NHL were prospectively enrolled, with median age of 70 years, DLBCL as the most common pathological subtype (64.4%), 8.9% of patients as the T-cell lymphoma, 18.8% of patients being indolent subtypes, 52.5% of patients having stage IV, 36.6% of patients showing high-risk IPI score, and the median percentage of M-MDSC among peripheral-blood CD45 + cells indicating 0.45%.
After a medium follow-up of 14.5 months, we confirmed that patients with higher percentage (>0.82%) of M-MDSC among peripheral-blood CD45 + cells had significantly worse overall survival (non-reach v.s. non-reach, P =0.011) when comparing to those with lower percentage (≦0.82%) of M-MDSC in PB.
With regard to the expression of TREM-2 on M-MDSC cell surface, M-MDSC from patients with aggressive lymphoma showed significantly higher normalized MFI change of surface TREM-2 when comparing to M-MDSC from patients with indolent lymphoma (Figure B); the normalized MFI change of surface TREM-2 on M-MDSC derived from patients with higher IPI scores is also significantly higher than those from patients with lower IPI scores (Figure C). Furthermore, patients whose M-MDSCs showed higher normalized MFI change of TREM-2 had significantly worse progression-free and overall survival than those with lower normalized MFI change of surface TREM-2 (Figure D & E).
To validate the clinical significance of TREM-2 on M-MDSC cell surface in adults with newly-diagnosed and treatment-naïve NHL, seven factors (age > 70 years, male gender, T-cell subtype, aggressive subtype, high-risk IPI score, percentage of M-MDSC among CD45 + cells in PB >0.82%, and normalized change of surface TREM-2 on M-MDSC >0%) were initially verified by univariate analysis and subsequently put into multivariate analysis if qualified, as shown by Table 1. At last, age (>70 years) and normalized change of TREM-2 on M-MDSC cell surface (>0%) were independent predictors of poor PFS and OS.
Conclusion:
For adults with newly-diagnosed and treatment-naïve NHL, patients with higher percentage of M-MDSC in PB is associated with worse prognosis; more importantly, high expression of TREM-2 on M-MDSC cell surface is an independent predictor for worse progression and overall survival. The functional role of TREM-2 on M-MDSC warranted further investigation for validating its possibility as an immunotherapeutic novel target.
No relevant conflicts of interest to declare.